Genetics and Cancer: Understanding the Role of Genes in Cancer Development
What are the specific genes that, when mutated, increase cancer risk?
Several genes, when mutated, can significantly increase the risk of developing cancer. These genes are often involved in critical cellular processes like DNA repair, cell growth, and cell division. Here are some of the most well-known ones:
Tumor Suppressor Genes:
- BRCA1 and BRCA2: These genes are involved in DNA repair. Mutations in these genes significantly increase the risk of breast, ovarian, prostate, and pancreatic cancers.
- TP53: This gene is known as the “guardian of the genome” because it plays a crucial role in regulating cell growth and preventing DNA damage. Mutations in TP53 are associated with a wide variety of cancers, including lung, breast, colorectal, and brain cancers.
- PTEN: This gene regulates cell growth and prevents cells from growing and dividing too rapidly. Mutations in PTEN are linked to an increased risk of breast, prostate, endometrial, and thyroid cancers.
- APC: This gene is involved in cell signaling and regulating cell growth in the colon. Mutations in APC are a major cause of colorectal cancer, particularly familial adenomatous polyposis (FAP).
DNA Mismatch Repair Genes:
- MLH1, MSH2, MSH6, PMS2: These genes are involved in repairing errors that occur during DNA replication. Mutations in these genes increase the risk of colorectal cancer, as well as other cancers like endometrial, ovarian, and stomach cancers. This is often associated with Lynch syndrome (hereditary non-polyposis colorectal cancer or HNPCC).
Other Genes:
- CDKN2A: This gene regulates cell growth and division. Mutations in CDKN2A are associated with an increased risk of melanoma and pancreatic cancer.
- RET: This gene is involved in cell signaling and development. Mutations in RET are linked to multiple endocrine neoplasia type 2 (MEN2), a condition that increases the risk of thyroid cancer and other endocrine tumors.
How do inherited genetic mutations differ from acquired ones in cancer development?
Both inherited and acquired genetic mutations can play a significant role in cancer development, but they differ in their origin, how they’re passed on, and their implications for cancer risk.
Inherited (Germline) Mutations:
- Origin: These mutations are present in the DNA of egg or sperm cells (germ cells) and are passed down from parents to their children at conception. This means every cell in the offspring’s body will carry this mutation.
- Transmission: Inherited mutations can be passed on from generation to generation within a family.
- Impact on cancer risk: Inheriting a cancer-related gene mutation significantly increases a person’s risk of developing certain cancers. However, it’s important to remember that it doesn’t guarantee cancer development.
- Examples: BRCA1/2 mutations (breast and ovarian cancer), TP53 mutations (Li-Fraumeni syndrome), APC mutations (familial adenomatous polyposis).
Acquired (Somatic) Mutations:
- Origin: These mutations occur during a person’s lifetime in the DNA of individual cells. They are not inherited from parents but arise due to various factors like:
- Errors during DNA replication
- Exposure to carcinogens (e.g., tobacco smoke, UV radiation)
- Random chance
- Transmission: Acquired mutations are not passed on to offspring. They are only present in the cells that developed the mutation and their daughter cells.
- Impact on cancer risk: Acquired mutations are the most common cause of cancer overall. The accumulation of multiple acquired mutations in a cell over time can lead to uncontrolled cell growth and eventually cancer.
- Examples: Most cases of lung cancer due to smoking involve acquired mutations in genes like TP53 and KRAS.
- It’s important to note that sometimes the same gene can be affected by both inherited and acquired mutations. For example, TP53 mutations can be inherited (leading to Li-Fraumeni syndrome) or acquired in various cancers.
- Understanding the difference between inherited and acquired mutations is crucial for:
- Risk assessment: Identifying individuals at higher risk of cancer due to inherited mutations.
- Cancer diagnosis and treatment: Identifying specific acquired mutations in tumor cells can help guide treatment decisions, such as targeted therapies.
What role do tumor suppressor genes play in preventing cancer?
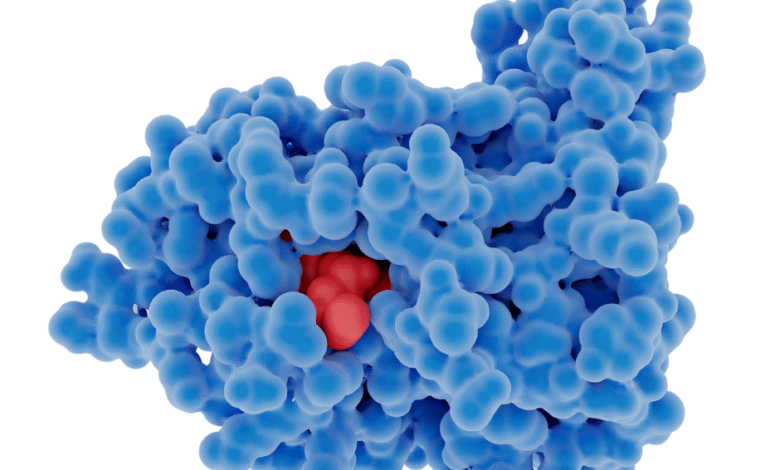
Tumor suppressor genes play a vital role in preventing cancer by regulating cell growth and ensuring that cells don’t grow and divide uncontrollably. They act as “brakes” on cell proliferation, preventing the formation of tumors. Here are the main ways they achieve this:
1. Controlling Cell Division:
- Slowing down cell cycle: Tumor suppressor genes produce proteins that regulate the cell cycle, the series of steps a cell goes through when it grows and divides. These proteins can slow down or halt the cell cycle if there are problems, such as DNA damage.
- Promoting cell differentiation: They encourage cells to mature and specialize into specific types of cells with defined functions. This prevents them from remaining in an immature, rapidly dividing state.
2. DNA Repair:
- Repairing damaged DNA: Some tumor suppressor genes are involved in DNA repair pathways. They help identify and fix errors that occur in DNA during replication or due to damage from external factors like UV radiation or chemicals. This prevents mutations from accumulating in cells, which can lead to cancer.
3. Apoptosis (Programmed Cell Death):
- Triggering cell suicide: If a cell is damaged beyond repair or has accumulated too many mutations, tumor suppressor genes can trigger apoptosis, a process of programmed cell death. This eliminates the potentially cancerous cell before it can cause problems.
4. Inhibiting Angiogenesis:
- Preventing new blood vessel formation: Some tumor suppressor genes can inhibit angiogenesis, the formation of new blood vessels. Tumors need a blood supply to grow and spread, so preventing angiogenesis can limit tumor growth.
What happens when tumor suppressor genes are mutated?
When tumor suppressor genes are mutated or inactivated, they lose their ability to control cell growth and division, repair DNA damage, or trigger apoptosis. This can lead to:
- Uncontrolled cell proliferation: Cells can grow and divide uncontrollably, forming tumors.
- Accumulation of mutations: Damaged DNA is not repaired, leading to a buildup of mutations that can further drive cancer development.
- Increased survival of abnormal cells: Cells with significant damage that should undergo apoptosis can survive and continue to proliferate.
How can genetic testing identify individuals at higher risk of certain cancers?
Genetic testing can play a crucial role in identifying individuals at higher risk of developing certain cancers by analyzing their DNA for specific inherited gene mutations. Here’s how it works:
1. Identifying Inherited Mutations:
- Focus on germline mutations: Genetic testing for cancer risk focuses on identifying inherited mutations (germline mutations) in genes known to be associated with increased cancer risk. These mutations are present in every cell of the body and are passed down from parents to their children.
- Analyzing DNA: Genetic tests typically involve analyzing a small sample of blood, saliva, or tissue for specific DNA sequences. These tests look for changes or mutations in genes that are known to increase cancer risk, such as BRCA1/2, TP53, APC, and others.
2. Assessing Cancer Risk:
- Positive result: A positive test result means that a person has inherited a mutation in a gene that increases their risk of developing certain cancers. The specific cancer risks associated with a particular mutation can vary depending on the gene and the specific mutation.
- Increased risk, not a diagnosis: It’s crucial to understand that a positive test result does not mean that a person will definitely develop cancer. It simply means they have a higher risk compared to the general population. The degree of increased risk can also vary.
- Negative result: A negative test result means that no mutations were found in the genes tested. However, it doesn’t eliminate the possibility of developing cancer, as most cancers are not caused by inherited mutations.
3. Guiding Prevention and Screening:
- Enhanced screening: Individuals with a positive test result may be recommended for enhanced cancer screening, such as more frequent mammograms or colonoscopies, starting at an earlier age.
- Preventive measures: In some cases, preventive measures may be considered, such as prophylactic surgery (e.g., mastectomy or oophorectomy) to reduce the risk of developing cancer.
- Lifestyle modifications: Lifestyle changes, such as maintaining a healthy weight, exercising regularly, and avoiding tobacco use, can also help reduce cancer risk.
Who should consider genetic testing?
Genetic testing for cancer risk may be appropriate for individuals with:
- A strong family history of cancer, especially multiple cases of the same type of cancer or cancer occurring at younger ages than usual.
- A personal history of certain cancers, such as breast cancer diagnosed before age 50 or ovarian cancer.
- A known family history of a specific gene mutation associated with cancer.
What are the ethical implications of genetic testing for cancer risk?
Genetic testing for cancer risk offers valuable information for individuals and families, but it also raises several important ethical considerations:
1. Informed Consent:
- Understanding the implications: It’s crucial that individuals fully understand the potential benefits, risks, and limitations of genetic testing before making a decision. This includes understanding the implications of both positive and negative results, as well as the possibility of uncertain results (variants of uncertain significance).
- Voluntary decision: The decision to undergo genetic testing should be voluntary and free from coercion.
2. Privacy and Confidentiality:
- Protecting genetic information: Genetic information is highly personal and sensitive. It’s important to ensure that genetic test results are kept confidential and protected from unauthorized access or disclosure.
- Potential for discrimination: There are concerns about potential genetic discrimination in areas such as employment, insurance, and social contexts. Laws like the Genetic Information Nondiscrimination Act (GINA) in the United States aim to protect individuals from genetic discrimination, but there are still limitations.
3. Psychological Impact:
- Emotional distress: Receiving a positive test result can cause significant emotional distress, anxiety, and fear. It can also impact family relationships and dynamics.
- Survivor guilt: Individuals who test negative for a mutation that runs in their family may experience survivor guilt.
4. Family Implications:
- Sharing information with relatives: Genetic test results can have implications for other family members who may also be at risk. There can be ethical dilemmas about whether and how to share this information with relatives.
- Duty to warn: In some cases, there may be a “duty to warn” relatives about a significant genetic risk, even if the individual who was tested does not want to share the information.
5. Access and Equity:
- Cost and availability: The cost of genetic testing can be a barrier for some individuals, and access to genetic counseling and testing services may not be equally available in all areas.
- Equity in access: It’s important to ensure that genetic testing is accessible to all individuals who could benefit, regardless of their socioeconomic status or background.
6. Variants of Uncertain Significance (VUS):
- Interpreting uncertain results: Sometimes genetic testing identifies a variant in a gene, but it’s unclear whether that variant increases cancer risk. These are called variants of uncertain significance (VUS). This can cause anxiety and confusion for individuals and their healthcare providers.
Can gene therapy be used to correct cancer-causing mutations?
Yes, gene therapy holds significant potential for correcting cancer-causing mutations. Here’s how it can be applied in cancer treatment:
1. Replacing Faulty Genes:
- Tumor suppressor genes: As discussed earlier, tumor suppressor genes normally prevent cancer by controlling cell growth, repairing DNA damage, and triggering apoptosis. When these genes are mutated, they lose their function, increasing cancer risk. Gene therapy can introduce a healthy copy of the tumor suppressor gene into cancer cells, restoring its function and helping to control cancer growth. A prominent example is the TP53 gene, which is mutated in many cancers. Gene therapy can be used to deliver a functional TP53 gene into cancer cells, potentially halting their uncontrolled growth.
2. Inactivating Oncogenes:
- Oncogenes: These genes promote cell growth and division. When they are mutated, they can become overactive, driving uncontrolled cell proliferation and cancer development. Gene therapy can be used to silence or inactivate these oncogenes, thereby inhibiting cancer growth.
3. Gene Editing:
- CRISPR-Cas9 technology: This revolutionary gene-editing tool allows scientists to precisely target and modify specific DNA sequences within cells. CRISPR can be used to correct cancer-causing mutations by directly editing the faulty gene sequence. This approach has shown promise in preclinical studies and is being explored in clinical trials.
4. Enhancing Cancer Immunotherapy:
- CAR T-cell therapy: This type of immunotherapy involves genetically modifying a patient’s own immune cells (T cells) to recognize and attack cancer cells. Gene therapy is used to introduce a new gene into the T cells that encodes a chimeric antigen receptor (CAR), which allows the T cells to specifically target cancer cells.





